Improve upstream RCM to achieve better documentation accuracy, less coding errors and minimized chances of denial risks with Denials 360. Claim denials significantly affect the financial and operational efficiency of the healthcare industry. According to a survey conducted by the American Hospital Association, nearly $19.7 billion is spent on overturning denial claims.
This is the major reason why a notable amount of healthcare industries is implementing proactive denial prevention that offers advanced platforms for improved code accuracy and documentation, along with better payer compliance.
Looking for proactive denial prevention? Denials 360 is the ultimate solution for you to upstream your revenue cycle and fix problems before claims. This platform maintains documentation integrity by analyzing claims for medical necessity, DRG accuracy and coding.
Let’s dive deep to study how integrating Denials 360 transforms denial management and creates a strong foundation for upstream RCM success.
Common Denial Triggers
Denial triggers in healthcare occur randomly. It is important to understand their root cause so that denial prevention in healthcare can be implemented to avoid such attacks.
Here is a breakdown of the most common denial attacks:
- Missing or wrong clinical information in the documentation
- Coding-related errors in diagnosis-related groups
- Compliance issues of payers
- Documentation gaps in medical necessity
- Authorization gaps in a submitted claim
Here is a chart below that illustrates the most common claim denials across the revenue cycle.
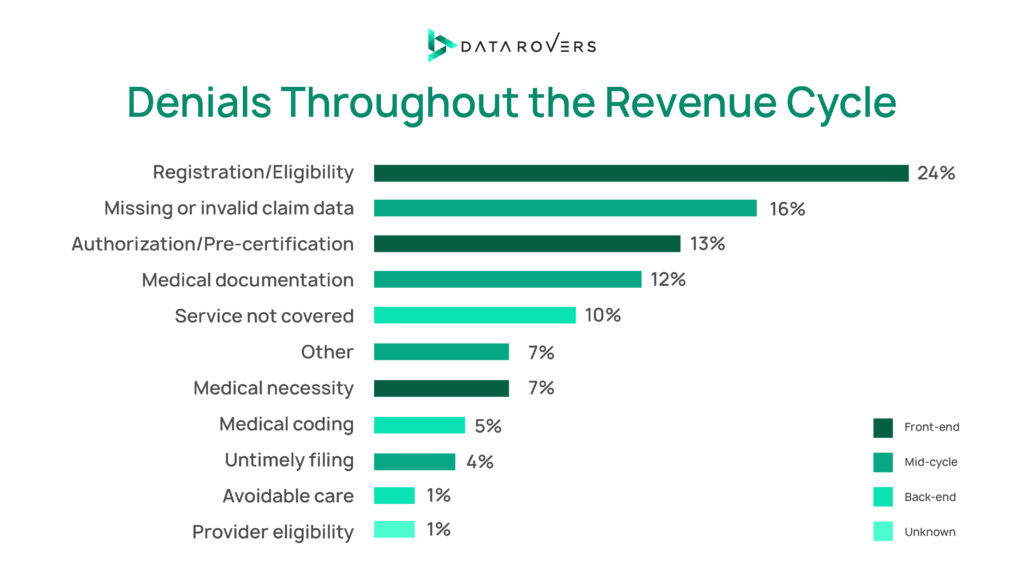
According to Optum 2024 Revenue Cycle Denials Index , Frontend and Backend RCM cause most denials, and it is highly recommended to have actionable insights to drive denial prevention strategies to avoid these denials as prevention is the key to prevent revenue loss. Understanding whether the denials are avoidable,recoverable and non- recoverable ,enable Revenue Cycle Management teams to prioritize strategically the goals such as maximizing potential reimbursements alongside actual reimbursement. Thus, investing in tools for proactive denial management in medical billing and revenue cycle management is a smart act.
✅ Ready to prevent denials before they start? Explore how Denials 360 ensures clean claims maintaining clinical documentation integrity. Schedule a Demo Now
Upstream RCM Vs Downstream RCM: Learn the Difference
To plan and implement effective denial prevention in healthcare, let’s understand the difference and impact on processes caused by upstream and downstream RCM.
What is Upstream RCM?
Upstream RCM includes all front-end processes that have an impact on data completeness and accuracy. Upstream RCM is essential as issues are identified in the upstream cascade to downstream denials.
Upstream RCM Processes Promoting Reimbursement Success
Documentation
Accurate and complete clinical documentation ensures complete medical necessity. It further reduces the chances of denial risks and claims.
Patient Registration
It is the initial step to prevent denial claims. Correct demographic information and insurance details to avoid the chances of unnecessary errors.
Coding
Translate the documentation into code. Errors in this process lead to underpayments, making it most crucial for maximum reimbursement.
What is Downstream RCM?
Downstream RCM includes all post-submitted tasks and usually contains the errors that were made in upstream RCM.
Downstream RCM Processes Promoting Reimbursement Success
Billing
Coded data is converted into financial claims, accuracy is vital in this process so there are no errors in the charges.
Tracking of Reimbursement
Monitors unpaid claims, delays and denials and aids in recovering lost revenue.
Submission of Claims
Sends finalized claims to insurance providers, and an error-free submission is significant for a quick reimbursement timeline.
Denial Management
This step occurs at the end and is crucial for loss management, better claim accuracy and have the revenue cycle management process closed accurately. It identifies the root cause of the denial claims such as coding errors, and inaccuracy in documentation.
💡Fact: According to the Health Financial Management Association, nearly 90% of denials can be prevented if identified in upstream RCM.
Understanding Clinical Documentation Integrity (CDI)
Clinical Documentation Integrity (CDI) refers to the process of ensuring that the clinical information is accurate and complete. CDI information is essential to correctly handle the reimbursement, medical reports, and compliance.
According to a survey conducted by the Association of Clinical Documentation Integrity Specialists, nearly 86% of the hospitals that implemented CDI observed better revenue and documentation quality.
Significance of Proactive CDI
Proactive CDI focuses on resolving the issues before claims denials are identified. They are more efficient as compared to reactive CDI.
Proactive CDI results in:
- Better code and reimbursement accuracy
- Less expensive than reactive CDI
- Promotes clean claims by reducing rework
- Enhances data quality
By shifting to Proactive CDI, healthcare organisations will have better clinical and financial performance. It also facilitates a better Case Mix Index (CMI).
Feature Overview: Denials 360
Denials 360 is an AI-powered denial management software that helps RCM teams actionable data insights with smart visuals integrated within the platform. It helps identify denial root causes to streamline the workflow by claim prioritization. RCM teams have the opportunity to prevent denials by analyzing claims related coding, medical necessity and DRG upgrades before submission. Gen AI capabilities make this platform unique as it provides a unified work management system to RCM professionals, so they work on real opportunities to collect potential revenue from payers. This platform assists in achieving higher clear claims and reduces administrative burden.
Core Features of Denials 360 for Denial Prevention
Claim Criteria Reviewer
This feature powered by Gen AI analyses the claims for clinical data and ensures the information is correct and complete, thus minimising the efforts on manual checks and unnecessary errors.
This feature analyzes for Medical Necessity, DRG and Coding related errors to prevent denials by maintaining Clinical Documentation Integrity (CDI).
Medical Necessity Validator
This feature makes use of artificial intelligence to validate the procedures against the payer-specific medical necessity guidelines.
DRG and Coding Errors Identifier
AI evaluates the data and ensures the clinical data is valid for accurate DRG. It identifies the inconsistency before the payers face the errors resulting in reduced cost audits.
Real-Time Updates and Feedback
Denials 360 has a proactive alert center where users immediately get notified of any specific alert generated across the teams. It further monitors the updates that directly edit the claim.
Want to learn more? Schedule Your Personalized Demo Now .
Let’s Find Out How Denials 360 Supports the RCM and CDI Team
Denials 360, an ultimate solution for claims denial management, is a game changer for everyone who is involved in the revenue management team. It automates their tasks, transforms their workflows and reduces the chances of inaccuracy in their work.
Denials 360 benefits for Clinical Documentation Integrity specialists in revenue cycle management
- Provides them with real-time policy updates
- Alert center for internal team communication
- Provides them access to claim analyzer
- Automatically corrects the deficiencies in the documentation
- Identifies the missing keys in clinical indicators
Denials 360 benefits for Revenue Cycle Management teams
- Predicts the patterns that might cause denials
- Monitors the claim rates and denial types
- Optimizes resource management to improve processes
With the help of Denials 360, you can use live data to track the causes of denial and payer requirements. It further sets predictive analytics on data errors and Gen AI to analyze documentation gaps. Denial Management Platform facilitates the generation of data-backed reports in order to guide your teams to focus on what matters the most.
Here are a few benefits Denials 360 has for healthcare teams:
- All updates and compliance are the latest and according to the guidelines
- It reduces the chances of human error
- No delays in payer changes
- Denial risk factors are minimized
According to a study conducted by the Healthcare Financial Management Association, nearly 35% to 65% of claims denials can be avoided by correct and accurate documentation.
Conclusion
Claim denials in healthcare are a significant challenge for the healthcare industry that can be prevented by implementing Denials 360 while improving the proactive CDI. This platform facilitates faster payment, enhanced documentation and reduced denial claims, thus helping CDI specialists, RCM Professionals and Healthcare Finance leaders. When documentation is accurate, risks of coding errors are minimized and repetitive work is avoided, the operational and financial performance is eventually improved.
👉Visit Denials 360 to transform your CDI today & recover potential reimbursement from payers!