Denied! The State of Claims in 2024
Experian Health’s survey of 210 patients and providers shows that claim denials are still a big problem in 2024. The survey found that 38% of claims are denied at least 10% of the time. It means it is a regular problem. The survey also found that 11% of claims are denied 15% or more of the time which shows that some claims face denials even more often. All of this suggests that claim denials remain a major issue, and the system needs improvements in the process. However, the advent of artificial intelligence (AI) shows huge potential in addressing this challenge. AI denial management software or platform integration into revenue cycle management (RCM) can help healthcare organizations proactively predict and prevent claim denials. As a result, they will streamline processes and enhance efficiency.
But, to check how true these statements are, we will analyze the manual processes of denial management with AI denial management platform processes to find out how effective it is in tackling these challenges to bring change.
What Is Denial Management in Healthcare?
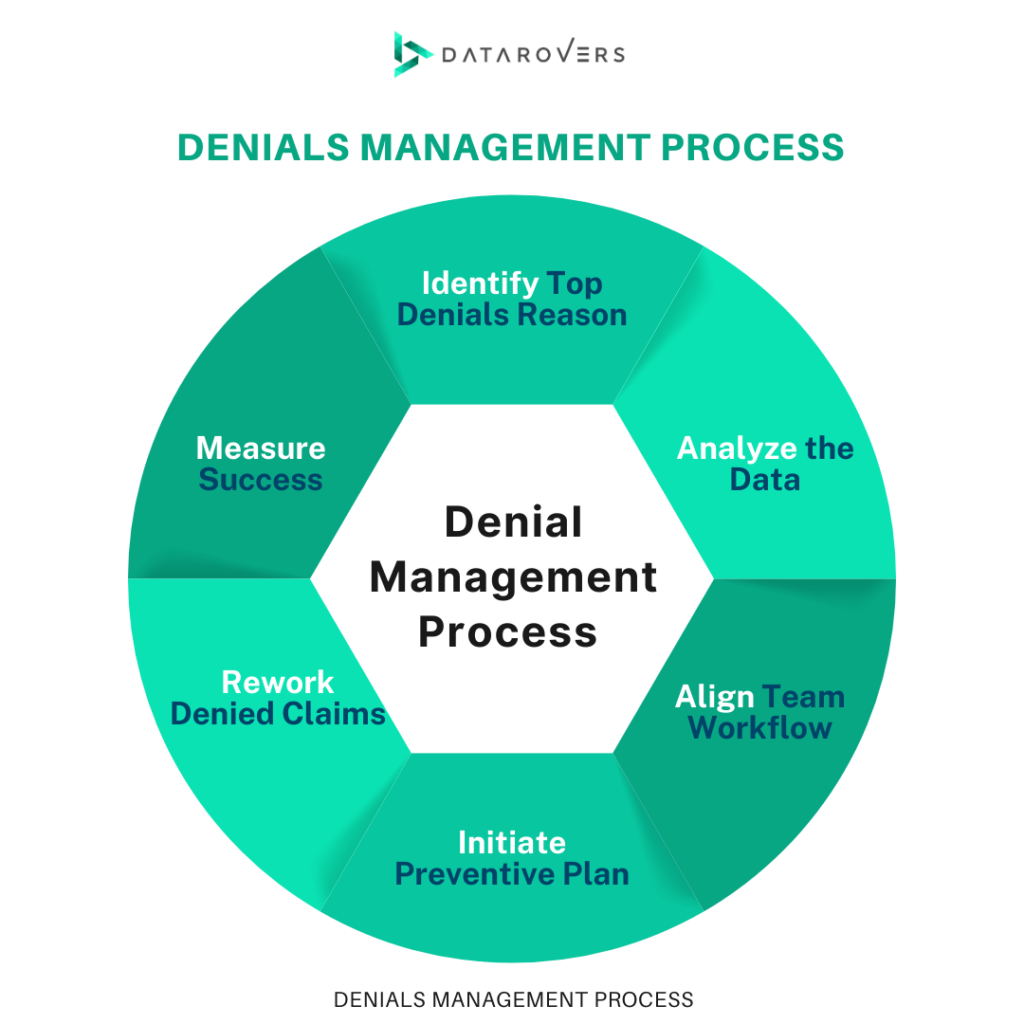
Denial management in healthcare is a process in which staff has to examine, correct and prevent claim denials. The denial management process involves steps like identifying top reasons for denial, analyzing data, aligning team workflow, discovering preventives, planning denial prevention, reworking denied claims and measuring success.
It happens when a payer from a specific insurance company denies a provider’s request for reimbursement of medical services already provided. Therefore, denial management is a continuous process requiring healthcare organizations to resolve front-end process issues for constant denial prevention.
Manual Processes of Denial Management in Healthcare
The traditional process of claim denial management is manual which is time-consuming and complex. More common issues are late submissions, lack of coverage by payers, missing information, and coding mistakes that cause claim denials. The reasons for these denials are mostly human errors, inefficient data management, or poor communication between healthcare providers and payers. Such inefficiencies can delay payments and require extra time and resources to resolve which also puts strain on administrative teams. Let’s see what a manual process of denial management process typically involves:
- Examine Denial Reasons: The team identifies the root cause of denials. It could be missing data, late submissions, or incorrect coding. Then, healthcare providers carefully review the reason codes provided by payers to understand the specifics of each denial. For that, they collect data to find out denial reasons. Providers then develop targeted strategies to address them and reduce recurrence. They identify patterns manually as it helps in allocating resources efficiently. It also ensures that the most common issues are addressed first.
- Analyze Denial Causes: Providers analyze patterns and then they develop strategies to avoid repeat denials. It includes correcting coding errors or ensuring timely submission. They have to use analytics to identify recurring issues, whether they stem from the payer’s side or the healthcare provider’s processes. This is mandatory to review denied claims regularly. Otherwise, it leads to denials. Detailed analysis helps uncover areas for staff training to prevent errors in the first place.
- Categorize Denials: Providers classify denials such as soft denials, hard denials, preventable, and clinical denials to streamline corrective actions. This categorization of denials allows teams to prioritize claims that require more immediate attention. For example, hard denials need an appeal. They also become aware of the denials that have significant impact on revenue and resource allocation. This classification also aids in improving workflows by correcting teams to handle the most pressing cases.
- Resubmit Claims: When issues are corrected, staff resubmit claims for payment. However, many denials can be reversed with proper action. Resubmission is an opportunity to recover revenue that might otherwise be lost, especially when the denial is due to a minor issue. However, many organizations fail to resubmit claims due to a lack of staff or systems to manage the process effectively.
- Track Results: The team monitors the progress of resubmitted claims to check if deadlines are met and no claims are left unresolved. These resubmitted claim tracking help healthcare providers meet the payer’s deadlines and avoid further penalties. This is a manual process so every time a resource has to be dedicated to act as a tracking system to prevent claims from falling through the cracks. It allows teams to follow up on pending claims and maintain transparency in the workflow.
- Create Preventative Mechanisms: Analysis helps in developing strategies and systems to prevent future denials by addressing issues. Moreover, preventing denials is the ultimate goal of an effective denial management process. Healthcare organizations review trends and implement corrective actions to minimize the risk of future claims being denied. This continuous training makes data management better which reduces errors and improves overall claim approval rates.
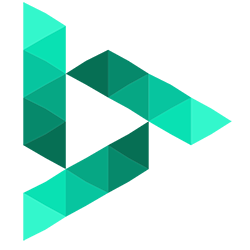
How Denials360 Transforms Manual Denial Management into an Automated Workflow?
Manual processes for claim denial management in healthcare are slow, expensive, resource-heavy, and prone to human error. However, Denials360 by DataRovers offers a solution to automate and optimize hefty processes. It significantly enhances efficiency and reduces costs. It possesses AI-powered capabilities to find the root cause to improve overall revenue cycle performance:
- AI-Powered Smart Queues for Triage
Denials360 is an AI denial management platform that helps reduce manual sorting and prioritization of claims by introducing AI-powered smart queues. It uses a proprietary claim scoring system which helps the platform automatically prioritize claims based on their financial impact. As a result, it ensures that the most important claims are addressed first. This automated triage process helps teams focus on high-value claims. Ultimately, it saves time and improves efficiency while reducing the risk of delayed claim resolutions.
- AI-Driven Claim Scoring and Forecasting
Denials360 is built on machine learning models which predict claim outcomes and identify potential underpayments before they happen. The AI claim scoring system helps providers spot at-risk claims, forecast approval chances, and detect DRG underpayments early. This helps healthcare providers recover more revenue and optimize their claims process.
- Real-Time Alerts and Instant Insights
Denials360 provides real-time alerts which notify providers when claims are denied. It allows them to take action without delay. The software generates AI-powered visual insights for healthcare teams to make informed decisions. This automated real-time insights notification minimizes the time spent on manual follow-ups and claims are resolved faster.
- Optimized Appeals Process
Traditionally, generating appeals for denied claims is time-consuming and error-prone because of manual intervention. Denials360 auto-fills case details and generates customized appeal letters based on the specific reasons for the denial. As a result, there is a streamlined approach to get higher recovery rates and better resource utilization.
- Workflow Efficiency and Resource Optimization
Denials360 has intelligent smart queues to help ensure task distribution on priority. This reduces administrative burden, improves productivity, and allows teams to focus on resolving complex issues rather than routine tasks.
- Data-Driven Decision Making
Traditional workflow decision-making is based on incomplete or subjective data. However, Denials360 uses AI-generated visualizations to offer data-driven insights into claim statuses, trends, and patterns. These insights empower healthcare teams to make faster, more informed decisions. Ultimately, it improves the accuracy and speed of the denial resolution process.
Get an AI Denial Management Software!
The challenges of manual management of claim denials show that it is inefficient and unsustainable for healthcare providers. The Denials360 is powered by Generative AI and Machine Learning which automates key denial management tasks, from triage to root cause analysis, appeals, and real-time alerts. It helps reduce manual errors and improves decision-making. Resulting in an optimized revenue cycle and recovery of lost revenue faster. Don’t let denied claims hurt your bottom line, get Denials360 now to transform your denial management and boost your financial performance.
Last Words
Manual workflows are a root cause of denied claims. Automated workflow of the entire denial management can transform healthcare organizations’ claim denial management. All AI-powered features streamline claims processing, reduce administrative overhead, prevent future denials, and optimize revenue cycle management. This AI solution not only increases efficiency but also maximizes revenue recovery by addressing issues proactively and providing real-time insights. If you are a healthcare provider looking to improve the claims process, get Denials360 to end the cycle of denied claims.