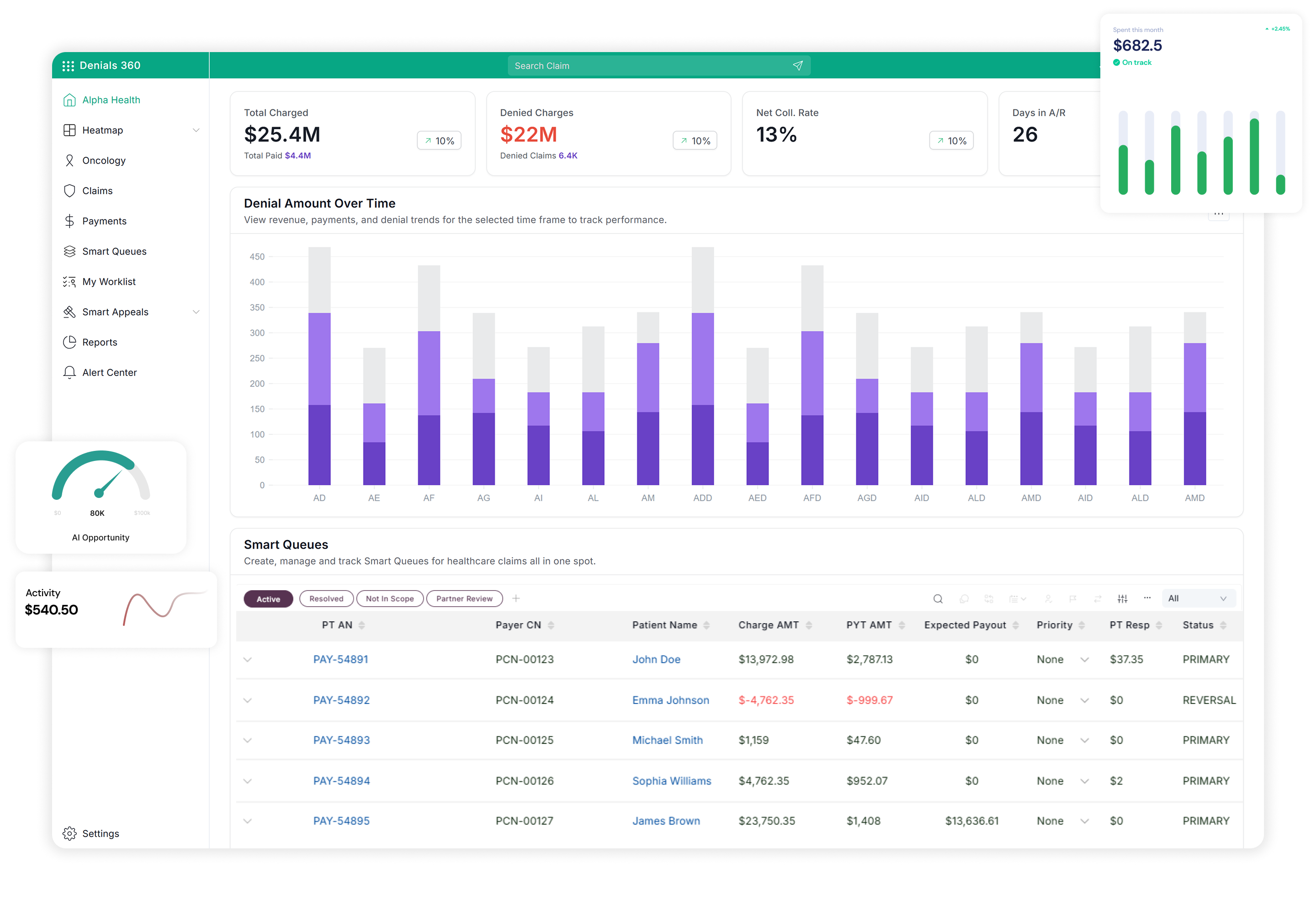
Increase your team’s efficiency 5X with tools built for speed and accuracy with real-time dashboards, smart triage rules, continuous policy updates, and one-click appeal automation.
End to End Denials Management Platform
Denial Management Software
Skip the IT wait—create stunning visuals instantly with generative AI!
Transform denials data into clear, actionable insights with Gen AI Data Smart Visualization, empowering your team to focus on what truly matters the most

Denial Management Software
Stay Ahead of Denials – Act Before They Happen!
Empower your team with real-time insights and advanced machine learning algorithms that predict claim outcomes, enabling you to spot and correct mistakes before submission. Prevent revenue loss, identify denial patterns, and drive smarter, proactive decision-making with data at the core.
Denial Management Software
Maximize Impact, Minimize Effort.
Streamline your workflow by focusing on claims with the highest payment potential, including DRG payments and resubmissions. Save time, reduce effort, and boost your team’s efficiency.
Denial Management Software
Smarter Workflows, Faster Resolutions.
Save valuable time for your revenue cycle team with automation powered by Smart Queues. Automatically triage denials and generate prioritized worklists, enabling your team to focus on resolutions that matter most.
Smart Appeals Software
Effortless Appeals, Seamless Resolutions.
Streamline your appeals process with Smart Appeals – an end-to-end solution for healthcare appeals. From generating appeal letters and prefilled payer forms to managing case files and supporting documents, we simplify every step for faster, more effective resolutions.
Smart Appeals Software
Streamline Appeals. Maximize Reimbursements.
Generate precise, AI-powered appeal letters in minutes. Our end to end appeals management solution automates medical necessity and DRG-based appeals, ensuring compliance, reducing denials, and improving claim success rates. With built-in criteria validation and seamless clinical note management, healthcare providers can recover more revenue with less effort.
Healthcare AI Copilot
Complex Policies, Simple Answers.
Say goodbye to navigating lengthy payer policies. Policy Copilot, powered by Gen AI, along with LUNA as its AI assistant providing policy updates, delivers instant and accurate answers to complex policy questions saving your team valuable time.

We Will Help You Achieve
90%
Denials Reduction
90%
First Pass Claim
30%
AR Reduction Rate
5X
Productivity Boost
5%-10%
Revenue Increase
Frequently Asked Questions
How do DataRovers ensure data protection and privacy of client’s information?
The DataRovers platform is fully compliant with HIPAA guidelines, and it provides end-to-end encryption and security for all data.
What is the pricing plan for each product or a complete solution suite?
Our pricing model ensures transparency, with no hidden charges. It’s based on your usage, determined by the quantity of claims, appeal letters, and inquiries you submit. Contact us for a quote today.
Can I have one of your solutions instead of taking all three?
Yes, you can pick the solution that compliments your business needs. Data Rovers is always happy to help you.
Talk to Our Experts
No More Revenue Loss Contact DataRovers for the Fastest Solutions!